Running Diabetes: The CGMS
[vc_row padding_top=”0px” padding_bottom=”0px”][vc_column fade_animation_offset=”45px” width=”1/1″][text_output]
I am Type 1 diabetic runner. That means I am an insulin dependent individual which I receive in specific continuous doses via an insulin pump. I am not going to cover what diabetes is or the difference between the types and other general stuff here. There are plenty of really good information available, you can take a look at sites like The American Diabetes Association, JDRF (Juvenile Diabetes Research Foundation), WebMD, TuDiabetes, DLife, and others. Here I will like talk about how I manage my sugars and diabetes while training, running and racing. For that purpose, I have divided the topic into several segments, from basic, details, opinions all the way to some running details.
[/text_output][/vc_column][/vc_row][vc_row padding_top=”0px” padding_bottom=”0px”][vc_column fade_animation_offset=”45px”][text_output]
I have been very fortunate that as a Type one diabetic individual to have been using a CGMS (ContiniousGluclose Monitoring System) for some time. A CGMS will take a reading of your glucose on a frequent basis without the need to prick your fingers that often. There are some calibration inputs required that you will still need to do with your standard glucose meter, so if you think you can get rid of your meter, don’t. At least not just yet, as technology continues to improve and sensors last longer there will be less and less of it. But even with today’s technology, I went from having to take 8-12 times a day to just 2-3 on average to keep my sugar under somewhat control. The CGMS provides me with a truckload of daily data, so you need to be comfortable with looking at it and finding meaning from that data in the form of numbers, arrow indicators, and graphs.
There are at least three main elements for the CGMS:
1. Transmitter
2. Sensor
3. Reciever/Data Display
There have been at least 4 iterations of the sensors I have used. Starting with the 1st FDA approved GCMS integrated with the Medtronic Paradigm insulin pump (5 or 7) series. Even though I was not able to get into the few pilot programs, I was able to get one as soon as it came out to be used by the public.
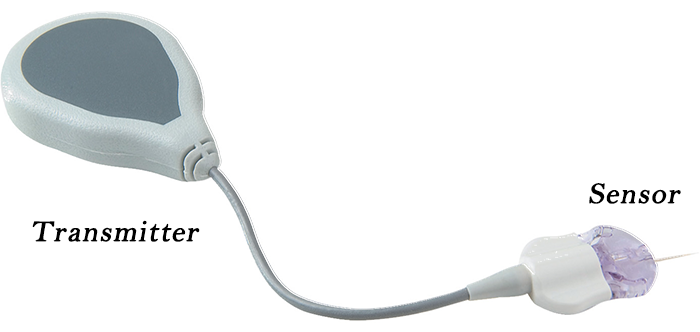
Continuous Glucose Monitoring System 1st generation integrated with the insulin pump
The transmitter was very massive and it required it’s own adhesive. The sensor worked accurately for about 4 days. But even those 4 days provided me with enough information to start making the adjustment and determining when to do the adjustments for food. This provided me with more freedom and actual control to understand how my body reacted to food, sickness, stress, sleep (or lack of it) and other. I also have to mention that at this time I was not putting the running mileage I am doing today. With that massive transmitter, I can imagine the transmitter coming loose during a long run due to the sweating and constant movement.
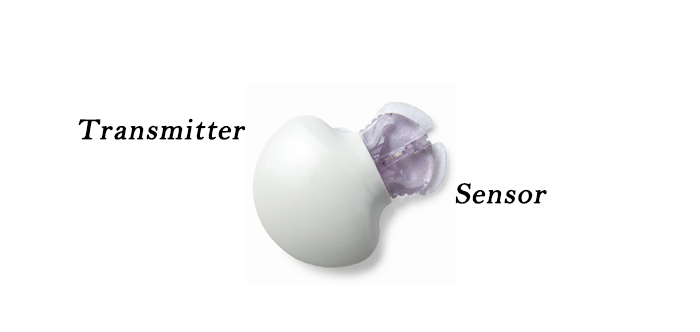
Continuous Glucose Monitoring System – 2nd and Enlite generation same form factor.
When the second generation came out it was with a smaller transmitter. So, the sensor and the transmitter will be together in one adhesive as a single unit. The third generation was same form factor and was called the Enlite sensor. That one lasted longer and was very accurate compared to the previous two generations. With this form factor, running is a breeze. The adhesive will hold the transmitter and sensor in place about 98% of the time.
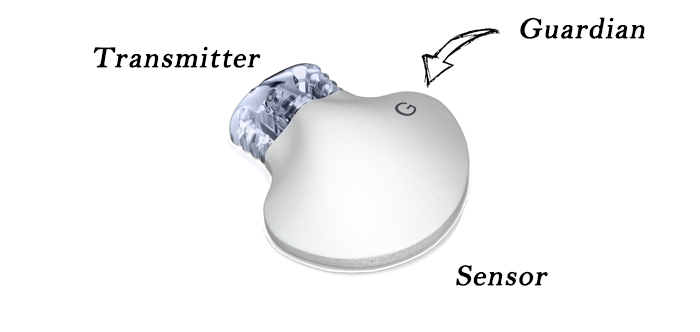
Continuous Glucose Monitoring (CGMS) Guardian generation integrated with the insulin pump
The most current generation is the Guardian. Again, same form factor, but this time the transmitter has a “G” that makes a distinction. This sensor last solid 7 days. It does integrate much better with the Medtronic 670G insulin pump as for the first time the pump will use the sensor information to make basal adjustments and minimized and stabilize the spikes of glucose highs and lows.
The CGSM sensor that I have used the most is the Enlite with the Paradigm Insulin Pump from Medtronic. It is the one that for me, lasted about 7 days (Adding an extra day after 1st change sensor notification). The CGMS will take a good solid day for the calibrations to take and the measurements to be very accurate. But even that day the information you get is very useful to manage and control your glucose. But for running, I try to get the best possible set of information that will help me keep my performance and a healthy activity going. I make sure that the new sensors change day is about two to three days prior to an event or key training run, especially a long run. I try to use steady/stable glucose readings for calibrations whenever I can. Now recently I started using the Guardian sensor also from Medtronic. Both sensors are well integrated with my insulin pump which makes it easy to manage and control. I will talk more about the readings trending and accuracy between the Enlite and Guardian sensors in a future post.
Typical Day:
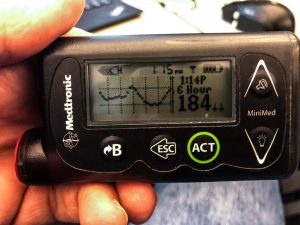 A typical day using the CGMS goes as follow; In the morning, normally before breakfast, I take a measurement with my meter to calibrate the sensor. I do any adjustment for sugars and carb intake when necessary. Throughout the day I will look at my pump and check the graph and lastest readings. From the graph, I will determine the glucose trending and the reading is the reference point to take any action. (The pump screen also provide trending information in the form of an arrow/s up or down is the measurement are moving in a predetermined fashion.) I like to use the graph and based on the information I will either do adjustments or check if it is in alignment with how I feel. (There have been occasions in which the sensor reading is off, but most of the time it is very close to what it should be) If how I feel does not match, I will take a glucose meter reading to check and calibrate if necessary, otherwise, no action is required. At night I try to do one calibration prior to the 12 hour calibration time line and then one close to the time I go to sleep. The reason for that extra calibration is that if the deadline was around 4:00 PM or 5:00 PM and I do not want the pump to wake me up to do a calibration, since the CGMS will ask for a calibration at 4:00 AM or 5:00 AM (or the equivalent of 12 hr of the last calibration) and that is a little bit annoying especially if you normally wake up later in the morning.
A typical day using the CGMS goes as follow; In the morning, normally before breakfast, I take a measurement with my meter to calibrate the sensor. I do any adjustment for sugars and carb intake when necessary. Throughout the day I will look at my pump and check the graph and lastest readings. From the graph, I will determine the glucose trending and the reading is the reference point to take any action. (The pump screen also provide trending information in the form of an arrow/s up or down is the measurement are moving in a predetermined fashion.) I like to use the graph and based on the information I will either do adjustments or check if it is in alignment with how I feel. (There have been occasions in which the sensor reading is off, but most of the time it is very close to what it should be) If how I feel does not match, I will take a glucose meter reading to check and calibrate if necessary, otherwise, no action is required. At night I try to do one calibration prior to the 12 hour calibration time line and then one close to the time I go to sleep. The reason for that extra calibration is that if the deadline was around 4:00 PM or 5:00 PM and I do not want the pump to wake me up to do a calibration, since the CGMS will ask for a calibration at 4:00 AM or 5:00 AM (or the equivalent of 12 hr of the last calibration) and that is a little bit annoying especially if you normally wake up later in the morning.
Sometimes (this is not recommended) when a calibration is needed and I do not have my meter accessible, I will look at the information from the reading and trends, compare that with how I am feeling and decided or not to fully trust the reading and use a projected/estimated glucose to enter for calibration purposes. If not, I will wait until I get to my meter. Keep in mind that if you decide to wait for the CGMS it will stop display new glucose data as a safety feature since the sensor needs to be calibrated.
Running:
 During my run, especially the runs lasting more than 30-45 minutes, GCMS provides me with the extra freedom not to necessarily carry a meter with me and the necessary information to make an adjustment, take extra gels/fuel or set a temporary basal due to low trending sugar. The combination of the CGMS and the pump has greatly improved my ability to enjoy more running and concentrate more on the workout knowing that I can get a reading almost every time I want to.
During my run, especially the runs lasting more than 30-45 minutes, GCMS provides me with the extra freedom not to necessarily carry a meter with me and the necessary information to make an adjustment, take extra gels/fuel or set a temporary basal due to low trending sugar. The combination of the CGMS and the pump has greatly improved my ability to enjoy more running and concentrate more on the workout knowing that I can get a reading almost every time I want to.
For Race day:
 One thing I notice is that no matter what event it is, I always get nervous. That nervousness somehow affects my sugars, and sometimes the sensor will act up. But with a standard routine, I can control it better especially in the early hours of the morning and at least have a great or decent running start. Throughout the event, I have had a range of experiences with the CGMS reading. Most of the time the readings are good and accurate information, but there have been occasions in which the data do not match with how I was feeling at that moment. This caused me to be very careful about adjustments during an event, especially if the readings are higher than I want them. All this came from some somewhat bad experiences with some training run, but especially my Rock and Roll Marathon experience in 2014.
One thing I notice is that no matter what event it is, I always get nervous. That nervousness somehow affects my sugars, and sometimes the sensor will act up. But with a standard routine, I can control it better especially in the early hours of the morning and at least have a great or decent running start. Throughout the event, I have had a range of experiences with the CGMS reading. Most of the time the readings are good and accurate information, but there have been occasions in which the data do not match with how I was feeling at that moment. This caused me to be very careful about adjustments during an event, especially if the readings are higher than I want them. All this came from some somewhat bad experiences with some training run, but especially my Rock and Roll Marathon experience in 2014.
NOTE: Make sure that you do a calibration reading before the race. It will help you determine how to proceed with the subsequent pump GCMS readings.
Sensor location:
For years I had been using the sensor in my abdomen. Alternating every time from left to right side. Over the time I felt that the readings started to be off more often. I can’t explain why or the reason for this to start happening. During winter and cold months, the readings were off even more. Late last year, my diabetes education recommended for me to use my legs as a sensor. At first, I was concern about the tape holding the sensor and receiver during my long runs. Also, will the constant movement of the leg (Which is more movement than my abdomen.) will the reading change? Well, to my surprise, all those concerns slowly disappeared with every single run using my legs. Not only that but the reading are more accurate and very close almost every single time I was getting a calibration measurement.
 Conclusion:
Conclusion:
Since late last year, as I mentioned earlier, I have been using the new Medtronic 670G Insulin Pump with the new Guardian sensors. I have to say, I am even more surprised and pleased with the changes and improvements. The new system was improved with better integration and accuracy of the sensors with the pump, but more about that in an upcoming post. In the end, I have been very fortunate to have a CGMS and using it had helped me to continue training, running many events, stay with running streaks longer and enjoy life.
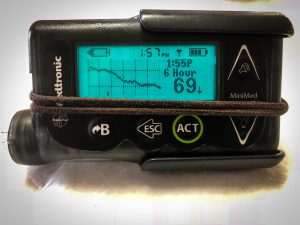
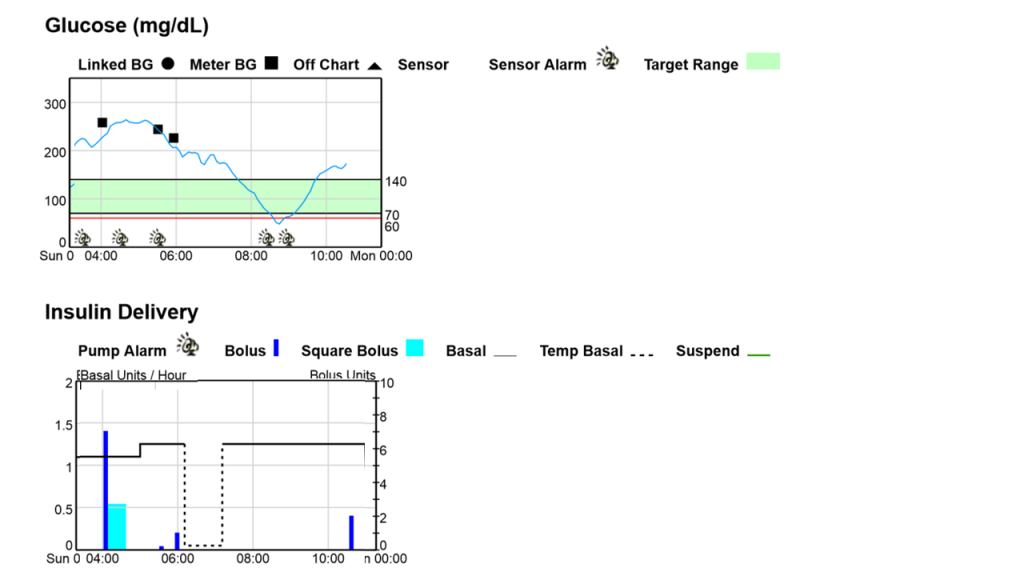
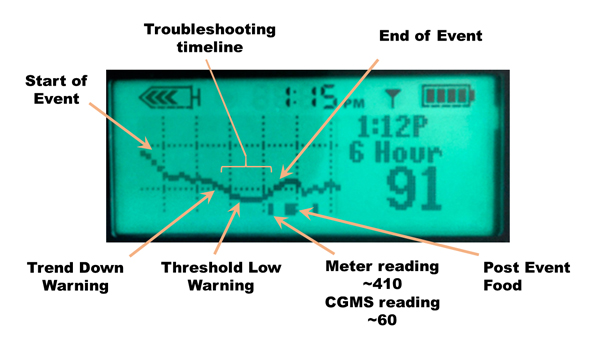
[/text_output][/vc_column][/vc_row][vc_row padding_top=”0px” padding_bottom=”0px”][vc_column fade_animation_offset=”45px” width=”1/1″][text_output]An example from 2016 City of Oaks Marathon event in which the CGMS was not accurate:
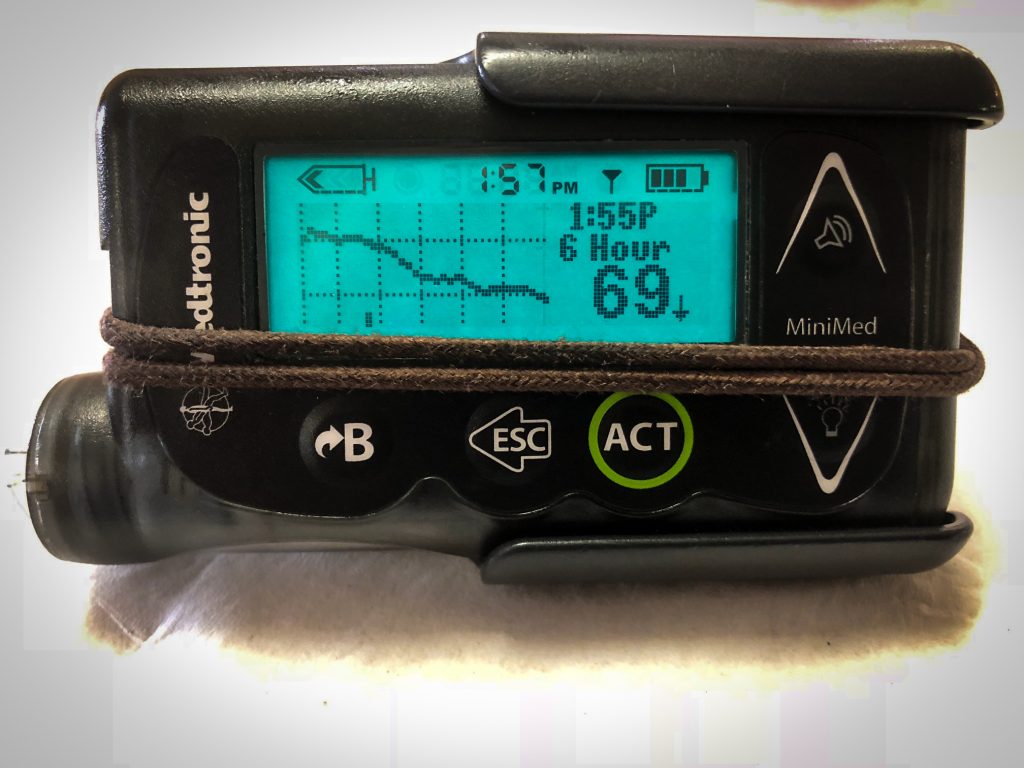
An example of a successful CGMS long event, Derby 50k. The sensor readings were spot on throughout the event:
 [/text_output][/vc_column][/vc_row]
[/text_output][/vc_column][/vc_row]